2Department of Pathology, Dhaka Shishu Hospital, Dhaka, Bangladesh
 10.3329/bmrcb.v44i2.38702
10.3329/bmrcb.v44i2.38702  0000-0001-9682-0844
0000-0001-9682-0844
Tribal population constitutes 1.8 percent of total population of Bangladesh. The study was conducted in the tribal population of Bangladesh to detect haemoglobinopathies and beta thalassemia trait. Another purpose of the study was to create awareness about thalassaemia and haemoglobinopathies among these indigenous groups. It was a cross sectional study conducted from September 2015 to November 2015. A total of 460 random samples were collected from three tribal groups, 175 cases from Chakma, 187 cases from Garo and 98 cases from Marma. Two cc of venous blood were collected in EDTA tube. Haemoglobin variants were studied by HPLC method using Variant Hemoglobin Testing System (Variant II Beta Thalassemia Short Program). Statistical analysis was carried out using SPSS statistical package (version 15). Data was analyzed by frequency distribution. Abnormal Haemoglobin variants were seen in 287 cases (62.4%) out of 460 cases and only 173 cases (37.6%) showed normal haemoglobin pattern. Haemoglobin E trait was the most common abnormality seen in 164 cases (35.6%) followed by Haemoglobin E disease which was seen in 101 cases (22%), Beta thalassaemia trait was seen in 22 cases (4.8%). This study shows a high percentage of Haemoglobin E trait and Haemoglobin E disease. Beta thalassaemia trait is also higher in comparison with randomly selected general population of Bangladesh. After calculating the estimate burden of child born per year by Harding Weinberg equation, it was to be found that the significant result which shows that 1552 new haemoglobin E beta thalassaemia and 22 new beta thalassaemia patients born per year in the tribal population. So, the tribal population should be properly screened and counseled for thalassaemia and haemoglobinopathies.
Keywords: Tribal population, Beta thalassaemia trait, Haemoglobin E trait, Haemoglobin E diseaseThalassemia and haemoglobinopathies are the most common congenital disorders in the world.1 Thalassemia have an autosomal recessive pattern of inheritance. Genetic diseases like thalassaemia are becoming an increasing health problem in developing countries as the deaths of children are falling due to better health services, vaccination against infectious diseases and improvement in nutrition.2 Although reliable data are still lacking from many regions of the world, recent data indicate that about 7% of the world populations are carrier of haemoglobin disorder and about 300,000 – 500,000 children are born each year with the severe homozygous states of these diseases.3
World Health Organation (WHO) data shows carrier status of Beta thalassaemia trait to be 3% and Hb E trait to be 4%. However, much of the data available from World Health Organization was based on studies that were carried many years ago and no regional data are available.3 Another study done in school children of different divisions of Bangladesh showed beta trait frequency 4.1% and Hb E trait 6.1%.2,4 This study also included frequency study of 44 tribal school children where 22% were found Haemoglobin E trait and 3% were found Beta trait.2
The total population of indigenous ethnic minorities in Bangladesh was estimated to be approximately 1.58 million out of 152.52 million total population in 2011 (last census) which represents 1.8% of total population.5 They comprise of diverse ethnic communities including Australoid, Tibeto-Burman and Sino-Tibetan races. Different ethnic groups of Bangladesh and their colorful lifestyles have significantly enriched the entire culture of Bangladesh.6 They are closely knit people marrying within their clans and therefore highly vulnerable to many hereditary disorders causing high degree of morbidity and mortality. As the frequency of thalassemia is increased by the consanguinity and endogamous mating, it may be assumed that the tribal communities are facing the problem at a very large scale. It is therefore very important to know their status of thalassaemia and haemoglobinopathies.
In Bangladesh, there are about 45 different tribal groups spread across the country.7 Chakmas are the largest ethnic group in Bangladesh. They live in Rangamati, Khagrachhari and Bandarban of Greater Chittagong Hilltracts, they also live in Teknaf of Coxsbazar. They are ancestor of mongoloid.8
Marmas are the second largest ethnic group. Majority of them live in Rangamati, Khagrachhari and Bandarban, some of them also live in costal area of Teknaf and Patuakhali.7 Marmas belong to the mongoloid races.9
Garopopulation is another large indigenous communities in Bangladesh.10 They live in the north-eastern part of Bangladesh, with the highest presence in the Gazipur, Mymensingh, Netrokona, Tangail, Sherpur, Jamalpur and Sylhet districts.11 There is no accurate information about the ancestosr of Garos. But anthropologists presume that Garos belong to the Tibet-Burmese people of the Mongoloid race.8
It was a cross sectional study. Study period was three months, from September 2015 to December 2015. Samples were collected from three major tribal groups Chakmas, Garos and Marmas. The samples were tested in Dhaka Shishu Hospital Thalassaemia and DNA Laboratory.
An educational session was given regarding thalassaemia and importance to know about carrier of thalassaemia and other haemoglobinopathies. The educational session also highlighted that marriage should be discouraged between carriers to prevent thalassaemia.
Sample collection and preparation: Two milliliters (2 ml) of venous blood was collected in a tube containing EDTA which were stored at 2–8 degrees Celsius and tested within three days. No preparation was required. HbA2/F calibrators and normal and abnormal controls were analyzed at the beginning of each run.
Variant Hemoglobin Testing System (Variant II Beta Thalassemia Short Program, Bio-Rad Laboratories Inc., Hercules, CA, USA) under the experimental conditions specified by the manufacturer.12
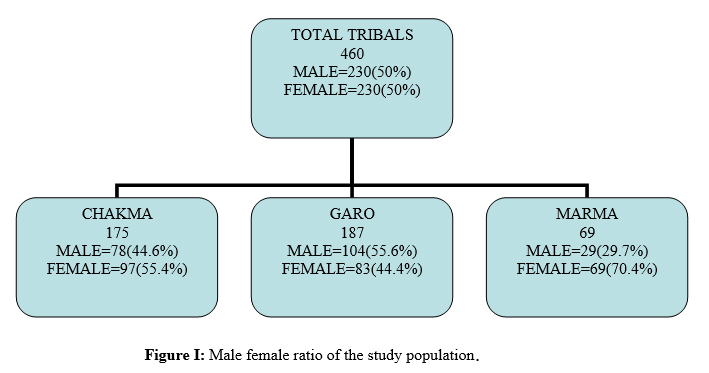
We collected 175 samples from Chakma Population, among them 78 cases (44.6%) were male and 97 cases (55.4%) were female, 187 samples from Garo population among them 104 cases (55.6%) were male and 83 cases (44.4%) were female, 98 samples were collected from Marma population among them 29 cases (29.6%) were male 69 cases (70.4%) were female. Total 460 samples were collected among them 230 cases (50%) were male and 230 case (50%) were female (figure: 1)
Out of 460 total tribal populations 22 cases (4.8%) were Beta thalassaemia trait, 164 cases (35.6%) were Haemoglobin E trait, 101 cases (22%) were Haemoglobin E disease, Only 173 cases (37.6%) showes normal haemoglobin varriant. Cumulative percentage of beta thalassaemia and Haemoglobin E trait and E disease were 62.4 % (table: I).
Status of Haemoglobins |
Sex |
Total |
|
|---|---|---|---|
Male |
Female |
||
Beta thalassaemia trait |
15(6.5%) |
7 (3.0%) |
22(4.8%) |
Haemoglobin E trait |
76(33.0%) |
88 (38.2%) |
164(35.6%) |
Haemoglobin E disease |
49(21.3%) |
52 (22.6%) |
101(22%) |
Normal haemoglobin varriant |
83(36.1%) |
90(39.1%) |
173(37.6%) |
Total |
230 |
230 |
460 |
Among 175 Chakma population beta thalassaemia trait were 10 cases (5.7%), Haemoglobin E trait were 59 cases (33.7%), Haemoglobin E disease were 22 cases (12.6%) and normal haemoglobin varriant were 84 cases (48%).
Among 187 Garo population beta thalassaemia trait were 8 cases (4.3%), Haemoglobin E trait were 70 cases (37.4%), Haemoglobin E dieasease were 71 cases (37.8%) and Normal haemoglobin varriant were 38 cases (20.3%).
Among 98 Marma population beta thalassaemia trait were 4 cases (4.1%), Haemoglobin E trait were 34 cases (34.1%), Haemoglobin E disease were 9 cases (9.2%) and normal haemoglobin varriant were 51cases (52 %) (table: II).
Reports of HPLC |
Chakma |
Garo |
Marma |
|---|---|---|---|
Beta thalassaemia trait |
10(5.7) |
8(4.3) |
4(4.1) |
Haemoglobin E trait |
59(33.7) |
71(37.8) |
34(34.1) |
Haemoglobin E disease |
22(12.6) |
70(37.4) |
9(9.2) |
Normal haemoglobin varriant |
84(48) |
178(20.3) |
51(52) |
Total |
175 |
187 |
98 |
It was seen that haemoglobin E disease were most common among Garos.
This study showed that there was high frequency of haemoglobin E trait and haemoglobin E disease in the tribal groups, beta thalassaemia trait was also little bit higher in comparison to the randomly selected general Bangladeshi population.
Result of the study showed 35.6% were heterozygous for haemoglobin E and 22% homozygous for haemoglobin E, cumulative percentage for haemoglobin E inheritance were 57.6%. A similar study in Indian tribals of Tripura showed Hb E carriers (45.8%) and homozygous E (14.83%). Chakmas who previously resided in Bangladesh showed 8 out of 9 children with HbE trait while the Jamatias also showed 8 carriers of HbE out of 9 children.13 Another study in the population of Northern Region of West Bengal reveals Hb E trait (34.4%) was most common followed by Hb E disease (25.3%).14 Hb E disorders (92.7%) were observed mostly among Rajbangsi population while E-β-thalassemias (40%) in the Muslims and a heterogeneous pattern noted among tribal and mongoloid.14
Hb E is common in the north-east India. About 50% Assam population have HbE and Tripura have 55% of Hb E which is similar in our tribal population. 15 While a previous study on school children of different districts showed carrier status of Hb E trait is 6.1% in randomly selected general Bangladeshi population.2,4 In the same study, a sample of 44 tribal children showed 22% Hb E trait in Chakmas.2
In this study, among 460 tribals, beta thalassaemia trait were seen in 4.8% while a previous study on school children of different districts showed carrier status of beta trait is 4.1% in Bangladeshi population.2,4 In the same study, a sample of 44 tribal children showed 3% beta trait in Chakmas.2
In this study, there was two cases with raised Hb F level and could be cases of Hereditary persistence of fetal Haemoglobin (HPFH) but needs to be confirmed by DNA analysis.16
With the result of the study applying Hardy-Weinberg Equqation we estimated 22 new cases of beta thalassaemia and 1552 new cases of haemoglobin E beta thalassaemia children birth per year in the tribal population, which is quite significant.
Conclusion
This study reveals that there was high frequency of Hb E trait and Hb E disease in the tribal population of Bangladesh and its coinheritance with beta thalassaemia trait will give birth to significant number of thalasaemic children in this population. The result in this study showed that a total of 1574 (Hb E beta thalasemia and beta thalassaemia major) children are born every year in this population. So, the tribal population should be properly screened and counseled for thalassaemia and haemoglobinopathies. They should be discouraged to marry between haemoglobin E trait and beta thalassaemia trait or between haemoglobinm E disease and beta thalassaemia trait. A large study needs to be done including all the tribal population in Bangladesh.
Acknowledgment
The study was funded by Bangladesh Medical Research Council. Dhaka Shishu Hospital Thalassaemia and DNA lab had supported to do HPLC and related laboratory works.
References
- Weatherall DJ, Clegg JB, Thalassemia-a global public health problem. Nat Med, 1996:2,847-9.
- Khan WA, Banu B, Amin SK et al. Prevalance of beta- thalassaemia trait and HB-E trait in Bangladeshi school children and health burden of thalassaemia in our population. DS (Child) H J, 2005;21:1-7
- World Bank 2006, report of a joint WHO-March of dimes meeting 2006.
- Old J, Angastiniotis M, Eleftherious A, Galanello, Harteveld C, Petrou M, et al. Prevention of thalassaemias and other haemoglobin disorder (2nd eds) Nicosia, Cyprus: Thalassaemia Intrnational Federation; 2013. p.137
- Statistics and informatics Division Ministry of Planning 2014, Population & Housing Census 2011, Bangladesh Bureau of Statistics, Dhaka.
- Ethnic Communities of Bangladesh. Kibriaul Khaleque From ‘‘Bangladesh - Land Forest and Forest People” - SEHD, Dhaka.
- BBS. 1991. Bangladesh Population Census 1991: analytical report, Bangladesh Bureau of Statistics, Dhaka, Bangladesh.
- Kamal, M, Islam Z & Chakma S (eds) 2007, Indigenous Communities, Asiatic Society of Bangladesh, Dhaka.
- Khan Sadat Ullah. ‘‘The Marma”. In Islam, Sirajul; Jamal, Ahmed A. Banglapedia: National Encyclopedia of Bangladesh (Second eds.). Asiatic Society of Bangladesh 2012.
- Islam M.R. 2008. The Changing Garo Adivasi Culture of Bangladesh: A Case Study of Marriage Rituals. M. Phil. Dissertation. Faculty of Social Sciences, University of Tromso, Norway
- Muhammed N, Chakma S, Masum FH, Hossain M, Oesten G. A CASE STUDY ON THE GARO ETHNIC PEOPLE OFTHE SAL (Shorea robusta) FORESTS INBANGLADESH International Journal of Social Forestry (IJSF), 2011,4:197-211
- VARIANT II b thalassemia short program instruction manual 2003.
- Sengupta B, De M, Dasgupta I, Poddar Set al. Comparative Study of Haemoglobinopathies in Tribal Populations of Arunachal Pradesh and Tripura (North East India). Int J Hum Genet, 2002;2:169-172
- Goswami BK, Pramanik R, Chakrabarty S, Pal PP, Banerjee S, Bandyopadhy A. Spectrum of Hemoglobin Variants in the Population of Northern Region of West Bengal: An Ethnogenetic Proposition. J Family Med Prim Care. 2014;3:219-223.
- Madhusnata De, Ajanta Halder, Sandeep Poddar, Rinni Sen, et al 2006. Anaemia and Haemoglobinopathies in tribal population of Eastern and North-eastern India, Heamatology.2006;11:371-373
- Amato A, Cappabianca MP, Perri M, Zaghis I, Grisanti P, Ponzini D, Di Biagio P 2014. Interpreting elevated fetal hemoglobin in pathology and health at the basic laboratory level: new and known γ- gene mutations associated with hereditary persistence of fetal hemoglobin. Int J Lab Hematol. 36:13-9