1Department of Neurology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
Background: Haematohidrosis is an extremely rare clinical condition in which the patient experiences sweat mixed with blood. Till date only a few cases of haematohidrosis have been reported in national and international medical journals. Pathogenesis of the condition is not yet established but rupture of the blood vessels of sweat glands due to activation of sympathetic nervous system from stress, anxiety or any other reason have been proposed as the cause of bleeding.
Objective: It was aimed to present the case who presented with episodes of sweat mixed with blood from different sites of her body.
Methods A case of haematohidrosis who experiences bloody sweat which comes with episodes of headache, was studied during in Bangabandhu Sheikh Mujib Medical University, Dhaka.
Results: Interestingly, it was to be found that a child of the patient, who is a 4 year old boy and a nephew of her, are suffering from the same condition. No family history was found in any of the previous cases. All other history and the investigations were insignificant. It was to be diagnosed the headache as migraine.
Conclusions: The patient was treated with propranolol and paracetamol. Her bloody sweat decreased significantly in both severity and frequency with the treatment.
Keywords:Hematohidrosis, Sweating blood, Headache, Migraine.Haematohidrosis, sometimes also referred to as haematidrosis, is an extremely rare clinical condition of sweating blood. Such phenomenon has long been associated with Christian religious belief, when Jesus Christ sweated blood before his crucifixion in the garden of Gethsemane. Instances are also found in the description of a legendary soldier by Leonardo Da Vinci who sweated blood before battle and there are also claims of such phenomena in some people awaiting execution.1 But only a few well documented case reports are available till now in modern medical literature.
Most of the cases are reported to have blood sweat with excessive exertion or anxiety. Reports are also available with otorrhoea and otoerythrosis, with epilepsy and with primary thrombocytopenic purpura.2-4
The exact pathogenesis behind haematohidrosis is not yet established. It is proposed that under pressure from sympathetic stimulation due to excessive stress or anxiety the vessels around sweat gland contracts. When the stress passes the vessels dilate to the point of rupture to cause blood being mixed with sweat. Here, it is reported that a case who presented with episodes of sweat mixed with blood from different sites of her body on the top of severe headache with strong family history of such condition.
A 25-year-old lady presented with episodes of headache which comes with sweat mixed with blood for 2 years. Her headache episodes were increased in both frequency and severity in last 2 months. Then, on an average she experiences 3 or 4 episodes of severe, dull aching headache in most of the days. These episodes were associated with photophobia and phonophobia. Headache usually starts in one side, mostly the left side of her head and neck and gradually spread over the whole of the cranium. At this stage, some headache episodes were associated with blood mixed sweat from different sites of her body through intact skin. This blood mixed sweat commonly comes from forehead, neck or hand and less commonly from scalp, chest or arms. She also had a few episodes of epistaxis and 2 episodes of bleeding from a scar of previous caesareaan section in her abdomen. The amount of blood was usually only a few drops. She remained drowsy after that for one or two hours. Then the headache usually subsides after the bloody sweatepis episode. Her menstruation was a bit irregular with occasional menorrhagia. No history of any previous bleeding manifestation was available. No drug history to mention expect occasional NSAIDs for headache.
The colour of tear, saliva, stool and urine was always normal. While exploring her family history, we astonishingly found that 1 of her 3 children, who was a boy of 4 years, was showing the same type of bloody sweat through intact skin for last 1 year. And another family member, who is son of her sister experienced the same.
Nothing significant was found from her general examination and all the systemic examinations. Thorough neurological examination including fundoscopy is also normal. She had such an episode of headache with bloody sweat while she was kept for observation in our hospital. The skin over the bleeding sites just after bleeding episodes was absolutely normal. There was no bleeding point or cut mark. Neither was there any tenderness or any other skin abnormality. The blood mixed sweat was bright red and appeared as ‘blood mixed with water or sweat’ in gross examination. It was unclotted when secreted but clotted on the intact skin as it was left there for a few minutes.



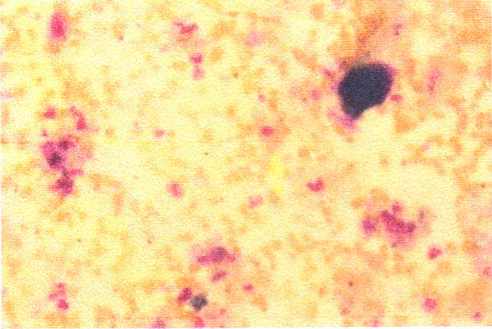
Everything was found normal after extensive investigations. Complete blood count showed mild normocytic normochromic anaemia with normal platelet count (Hb: 11.5 gm/dL, Platelet count: 275x109/L). Bleeding time and clotting time were normal (2 minutes and 30 seconds and 5 minutes 30 seconds respectively). Prothrombin time was 12 seconds (INR 1.01) and activated partial thromboplastin time was 30 seconds which were also within normal range. Other investigations including serum electrolytes, renal and liver function tests were also normal. Peripheral smear was prepared from the secretion with Lishmann stain, microscopic examination of which revealed numerous RBCs along with some WBCs and platelets with a few epithelioid cells (figure 4).
ABO blood group was also done taking samples from both venous blood and from bloody sweat. Both were found to be B positive.
For her headache she was treated as migraine. Acute episodes were treated with Paracetamol 1gm. As some previous reports showed that haematohidrosis episodes partially responded to beta blocker, Propranolol was started in low dose and increased gradually both as migraine prophylaxis and to cover haematohidrosis. With dose of Propranolol 40mg 12hourly, she showed significant improvement of headache. Bloody sweat episodes also declined to 1 episodes in 3 or 4 days after a few weeks of treatment.
The patient described here was an otherwise healthy female of 25 years who was experiencing severe headache along with bloody sweat for 2 years. Thorough clinical examinations and investigations were normal. There was no clue of any bleeding diathesis or any other systemic disease. All her bloody sweat episodes occurred on the top of severe headache. Some episodes occurred when she was in the hospital in front of attending doctors and nurses. Thus the chance of factitious disorder was excluded.
As an explanation for such phenomenon in previous cases, activation of the sympathetic nervous system has been implicated.5 It was proposed that multiple blood vessels present in a net-like form around the sweat glands. The vessels initially constricts with activation of sympathetic nervous system. As the sympathetic stimulus passes away the vessels dilate to the point of rupture. The blood goes into the sweat gland which is then pushed along with sweat to the surface presenting as droplets of blood being mixed with sweat. Then the vessels were collapsed leaving no scar on the skin. Extreme physical or emotional stress were most common causes for such activation. In this case severe headache is probably the cause of sympathetic activation. Other causes were ruled out by thorough history taking and examination.
Some tests like Benzidine test and Haemochromogen test could be performed to identify haemoglobin in the sample. In Benzidine test, haemoglobin reacts with hydrogen peroxide liberating oxygen. Oxygen then reacts with organic reagent and turns the solution green/blue. In this patient, these tests were not done as presence of numerous RBCs along with all other components of blood were visualized in microscopic examination. ABO and Rh typing was also done taking sample from bloody sweat which matches patient’s blood group. Thus the blood was confirmed to be originated from the patient’s own peripheral blood.
Immediate biopsy would show multiple blood filled spaces that open directly to the follicular canals or to the skin surface. After exudation, the blood vessels collapses and biopsy would not be helpful. Biopsy in this patient was not done as it was refused by the patient.
In this patient, we noticed strong family history of the condition. One of three of her children, and a nephew of her are affected. So far family history was not present in the previously reported cases.
Treatment was not yet very convincing. Remission of symptom with propranolol were commonly reported in patients with prominent features of sympathetic activation.6 Administration of Benzodiazepines to reduce patient’s anxiety was also found in some cases.5 Another report showed attenuation of symptoms with transdermal atropine patch.7 This patient was treated for her headache as migraine. Propranolol was given both as migraine prophylaxis and as treatment for haematohidrosis. The patient showed significant improvement of both her headache and bloody sweats.References
- Holoubek JE, Holoubek AB. Blood, sweat and fear. “A classification of hematidrosis”. J Med. 1996; 27: 115-33.
- Migliorini L. Hematidrosis otorrhea with otoerythrosis. Friuli Med. 1962;17:768-74.
- Shen H, Wang Z, Wu T, Wang J, Ren C, Chen H, Yu Z and Don W: Haematohidrosis associated with epilepsy in a girl successfully treated with oxcarbazepine: Case report. J Int Med Res 2015; 43: 263-69.
- Duan Y, Zhao X, Xu X, Yang J, Li Z. Treatment of Primary Thrombocytopenic purpura by Modified Minor Decoction of bupleurum. J Tradit Chin Med. 1995; 15:96-98.
- Manonukul J, Wisuthsarewong W, Chantorn R, Vongirad A, Omeapinyan P. Hematidrosis: a pathologic process or stigmata. A case report with comprehensive histopathologic and immunoperoxidase studies. Am J Dermatopathol. 2008; 30:135-39.
- Wang Z, Yu Z, Su J, Cao L, Zhao X, Bai X, et al. A case of hematidrosis successfully treated with propranolol. Am J Clin Dermatology. 2010; 11:440-43.
- Biswas S, Surana T, De A and Nag F. A Curious Case of Sweating Blood. Indian J Dermatol. 2013; 58: 478-80.

