Md Fakhrul Alam
Department of Paediatrics, Bangabandhu Sheikh Mujib Medical University, Bangladesh.
Mohammed Mahbubul Islam
Department of Paediatrics, Bangabandhu Sheikh Mujib Medical University, Bangladesh.
Mujammel Haque
Department of Paediatrics, Bangabandhu Sheikh Mujib Medical University, Bangladesh.
Shahana A Rahman
Department of Paediatrics, Bangabandhu Sheikh Mujib Medical University, Bangladesh.
Keywords: Juvenile Idiopathic Arthritis, Serum homocysteine levels, Polyarticular, Hyperhomocysteinaemia
DOI: 10.3329/bmrcb.v46i1.47463
Abstract
Background: Juvenile Idiopathic Arthritis (JIA) is the most common chronic rheumatic disease of childhood and a leading cause of short and long-term disability. Abnormal level of serum homocysteine (Hcy) may be found in Juvenile idiopathic arthritis (JIA) patients. Some studies were done on serum homocyestine levels in children with JIA which showed conflicting results. So far, no study regarding the Hcy level in JIA patients was done in Bangladesh.
Objectives: The study was aimed to assess the homocysteine level in children with different subtypes of JIA.
Methods: It was a cross sectional and case control study. Fifty newly diagnosed cases of JIA attending the Pediatric Rheumatology clinic of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, from January 2016 to March 2017 were included. Fifty age and sex matched controls were selected. Serum homocysteine levels were measured in both cases and controls.
Results: Among JIA patients, 36% had high serum homocysteine (Hcy) level whereas 100% of controls had normal level. Mean hcy level was significantly (p<0.05) higher among cases than controls. Significantly higher number and level of hyperhomocystaeinemia was found among JIA patients having duration of illness more than 1 year than duration less than 1 year. Mean homocysteine level of polyarticular RF positive cases was found as 14.38±3.79 µmol/L and that of SJIA was found as 13.0±4.66 µmol/L. When compared with homocysteine levels of control group these two groups had significantly higher homocysteine level.
Conclusions: More than one third of JIA patients had hyperhomocysteinaemia. Mean hcy level of JIA cases was significantly higher than that of controls. Significant association of hyperhomocysteinaemia was present with duration of illness and certain types of JIA.
Keywords: Juvenile Idiopathic Arthritis, Serum homocysteine levels, Polyarticular, Hyperhomocysteinaemia
Introduction
Juvenile idiopathic arthritis (JIA) is the most common rheumatic disease of children. JIA is characterised by idiopathic peripheral arthritis with an immunoinflammatory pathogenesis possibly activated by contact with external antigens. Worldwide incidence of JIA ranges from 0.8 to 22.6 per 100,000 children per year with the prevalence ranges from 7 to 401 per 100,000 children. JIA is classified into seven subgroups according to International league of association for rheumatology (ILAR) 2001 classification.1
Homocysteine (Hcy) is a sulphydryl amino acid derived from the essential amino acid methionine during its conversion to cysteine.2 Main metabolic pathway of Hcy requires folic acid, vitamins B6 and B12. Its concentration depends on age, gender and ethnic background.3 Homocysteine can impair bone health by interfering with osteoclastic activity. Furthermore, homocysteine induces apoptosis of human bone marrow stromal cells, thereby impairing bone repair.4,5 It is reported that an increased homocysteine level is a strong and independent risk factor for osteoporotic fractures in older people.5
Different genetic and acquired factors may lead to an elevated homocysteine level.6 Acquired factors are more common than genetic disorders, and include vitamin B12, B6 and folate deficiency and side effects of some drugs (methotrexate, phenytoin, carbamazepine and many more).7 As JIA is a chronic inflammatory disease, there could be some sort of multivitamin deficiencies specially vitamin B12, B6 and folate. There are some studies done on the level of Hcy in children with JIA but the results have been conflicting.8,9 No study is available in Bangladesh concerning JIA and homocysteine level. The aim of this study was to estimate the serum homocysteine level in different subtypes of JIA patients. Specific objectives were to compare the homocysteine level in different subtypes of JIA with controls, also assessed relationship between duration of disease at presentation with homocysteine level.
Materials and Methods
In this case control study, newly diagnosed fifty cases of JIA according to International League of Associations for Rheumatology (ILAR) attending paediatric rheumatology follow up clinic and peadiatric ward, BSMMU during January 2016 to March 2017 were included. Purposive sampling was done to meet the inclusion criteria. Patients were excluded if they had either an additional chronic disease (endocrine, neurological, cardiac, renal or liver disease) that could affect homocystine metabolism, or were receiving treatment including methotrexate or vitamins like B6, B12 and folic acid. Fifty age and sex matched controls were selected from the outpatient department who attended the hospital because of acute illness other than JIA or bone disease, and who were not taking supplements of any vitamins or folic acid. Ethical approval was obtained from the Institutional Review Board of BSMMU. Informed written consent was obtained from all the participants or parents. Information were obtained from their medical records, which included age, gender, duration of disease and disease sub-type according to the ILAR classification criteria.
With all aseptic precaution 2 ml venous blood samples were drawn for measuring homocyestine levels for both the cases and controls. Serum was separated by centrifugation within 30-45 mins of collection and was preserved in ultra-freezer at -20 degree centigrade after labeling. Serum homocyestine level was determined by chemiluminescence microparticle immune assay (CMIA) using the analyzser The Architect system Homocyestine assay, Abbot; Germany 2008 in the Department of Biochemistry, BSMMU. There are two studies about the level of Hcy in children with JIA and the results have been conflicting.8 Normal serum level of homocysteine in adults is usually 5-15 μ mol/l, with a mean level of 10µmol/l according to the standard methods.10 The levels of hcy between different types of JIA and different disease duration were compared in the present study. Hcy levels between cases and controls were also compared.
All statistical analyses were done using the statistical software SPSS 23.0. The Chi-square test, student t-test and scatter diagram was applied to evaluate the association between the variables when indicated. A p-value of less than 0.05 was considered as significant at a 95% confidence interval.
Results
It was observed that majority (44.0%) patients belonged to the age group of 11-15 years among the cases with a mean age 8.96±4.25 years (Age range: 1.0 year to 16 years). Majority (58.0%) patients were male among cases (table I). The mean age of controls was 9.72 years (Age range: 1.2 to 15 years) and among them 29 (58.0%) were male and 21 (42.0%) were female.
| Demographic variables | Case group (n=50) | |
|---|---|---|
| n | % | |
| Age (years) | ||
| ≤5 | 13 | 26.0 |
| 6-10 | 13 | 26.0 |
| 11-15 | 22 | 44.0 |
| ≥15 | 2 | 4.0 |
| Mean±SD | 8.96 | ±4.25 |
| Range (min-max) | 1.0 |
-16.0 |
| Sex | ||
| Male | 29 | 58.0 |
| Female | 21 | 42.0 |
| Male: female | 1.38:1 | |
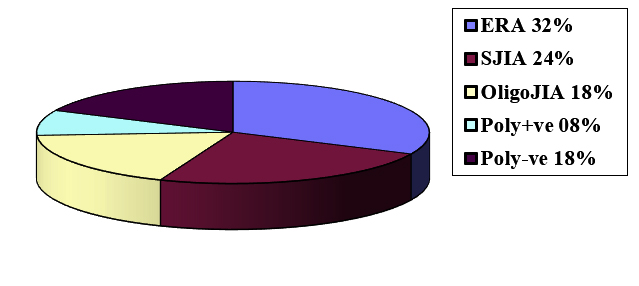
Five subtypes of JIA patients were found (Figure 1) including ERA (32.0%), systemic JIA (24.0%), oligo-articular JIA (18.0%), poly-articular RF negative (18.0%) and poly-articular RF positive JIA (8.0%). In the JIA group (cases), homocyestine level was normal in 64.0% and high in 36.0%. Among control group, all had normal homocyestine levels (table II).
| Level of homocysteine | Case (n=50) |
Control (n=50) |
p value | |||||
|---|---|---|---|---|---|---|---|---|
| N | % | n | % | |||||
| 5-15 µmol/L | 32 | 64.0 | 50 | 100.0 | 0.024s | |||
| >15 µmol/L | 18 | 36.0 | 0 | 0.0 | ||||
| Mean±SD | 11.43 | ±4.29 | 9.08 | ±2.28 | ||||
| Range (min-max) | 6.53 | -20.52 | 5.33 | -12.5 | ||||
The mean homocysteine level of cases was significantly higher than controls. High level of homocysteine was found in more than two-thirds (69.2%) of patients having duration of illness more than 1 year. This was statistically significant (Table III).
| Duration of illness | Level of homocysteine |
p value | |||
|---|---|---|---|---|---|
5-15 µmol/L |
>15 µmol/L |
||||
| N | % | n | % | ||
| <6 month (n=15) | 13 | 86.7 | 2 | 13.3 | |
| 6 month-1 year (n=22) | 15 | 68.2 | 7 | 31.8 | |
| >1 year (n=13) | 4 | 30.8 | 9 | 69.2 | |
| Mean±SD | 9.31 |
±5.61 | 13.36 |
±7.51 | 0.035s |
| Range (min-max) | 1.5 |
-24 | 2 |
-24 | |
s= significant
p value reached from chi square test
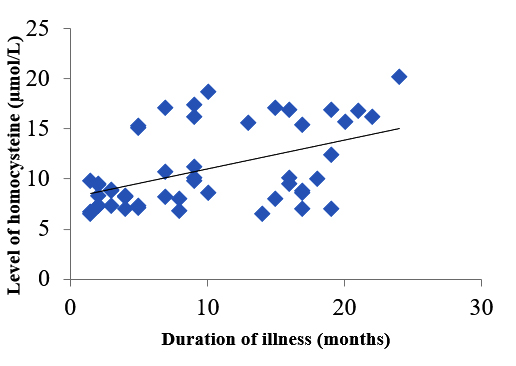
The scatter diagram showed that homocysteine levels increased significantly with the increased duration of disease at onset (Figure 2) Spearman correlation coefficient was: 0.476 which was statistically significant (p=0.001).
When compared with homocysteine level of controls, polyarticular RF positive JIA and systemic JIA patients had significantly higher homocysteine level (Table IV)
| Type of JIA | Level of homocysteine |
p value | |||||
|---|---|---|---|---|---|---|---|
Cases |
Controls |
||||||
| N | Mean | ±SD | n | Mean | ±SD | ||
| Oligoarticular | 9 | 11.65 | ±4.55 | 50 | 9.08 | ±2.28 | 0.051ns |
| Polyarticular RF positive | 4 | 14.38 | ±3.79 | 50 | 9.08 | ±2.28 | 0.001s |
| Polyarticular RF negative | 9 | 11.54 | ±3.99 | 50 | 9.08 | ±2.28 | 0.096ns |
| SJIA | 12 | 13.0 | ±4.66 | 50 | 9.08 | ±2.28 | 0.003s |
| ERA | 16 | 8.45 | ±2.38 | 50 | 9.08 | ±2.28 | 0.425ns |
s= significant, ns= not significant
p value reached from unpaired t-test
Discussion
Homocysteine (Hcy) is a sulphydryl amino acid derived from the essential amino acid methionine during its conversion to cysteine, which is a marker of severity of arthritis in JIA patients.2 Its concentration in the plasma or serum is about 10 μmol/L. A plasma homocysteine concentration exceeding 15 μmol/L is termed as hyperhomocysteinaemia in adults.10,11 Not much data exist on Hcy levels in children.10 One study found that Hcy levels in 8-12 year old boys and girls were about half of that found in adults.12 There was no sex difference and the Hcy distribution was nearly Gaussian, with a mean level of 5.25 µmol and the reference range was from 2.9 to 7.6 µmol . Another study showed that distribution of Hcy levels in children was substantially lower than that of adults.3
Few studies done on the level of homocysteine (Hcy) in children with JIA found conflicting results.8,9 But it is believed that there is a relationship between blood homocysteine levels and severity, duration and subtypes of JIA.8 Present study assessed the Hcy level of JIA patients and compared with controls in a tertiary care hospital in Bangladesh. Though it is assumed that the Hcy level in children is lower than that of adults; as no standard is available, this study considered adult standard to define hyperhomo-cysteinaemia.
Most of the cases (44.0%) were within 11 to 15 years age group which supports the juvenile onset of the disease. Among the cases, male: female ratio was 1.38:1. A prospective observational study carried out in the same set up also found more males than females (M:F ratio approximately 2:1), and most of the patients were in the age group of 11-15 years.13
This different result regarding sex distribution and types of JIA found in this study could be due to social or geographical difference. In the present study, maximum number of patients were suffering from ERA (32%), followed by SJIA, polyarticular and oligo articular JIA (Figure 1). This order of frequency probably reflects the higher attention to male children in our perspective. ERA was found as the predominant type in some other studies done in India and Taiwan as well.14,15
The present study is consistent with the study of Huemer et al (2003) where JIA patients had significantly higher level of Hcy than that of controls.8 Goncalves et al compared the plasma Hcy concentration between 51 JIA patients with 52 healthy controls. The mean plasma Hcy concentration was higher in JIA patients than in healthy controls (p = 0.615). Significantly higher concentration of Hcy was observed in the subgroup of 13 – 18 years (p < 0.001).16 As because, our study did not subgroup the JIA patients according to age, this comparison could not be done.
Association of homocysteine level with duration of illness was seen in the present study and it was found that 69% of JIA patients with disease duration more than one year at presentation, had hyperhomocysteinemia. No documented reports were available for comparison of this finding. But if the mechanism of hyperhomocysteinemia in arthritis is analyzed; it is found that there is reduction in circulating levels of pyridoxal 5`-phosphate (PLP), the biologically active form of vitamin B6 in rheumatoid arthritis. This low level of PLP ultimately raises the Hcy level.17 So, it can be extrapolated that, as duration of illness increases PLP level continues to decrease further which in turn increases the Hcy level.
Although the mean Hcy level was within the normal range, polyarticular seropositive JIA and systemic JIA patient’s Hcy levels were significantly higher than that of the controls. Perhaps it was due to the natural history of the serotypes having worst disease course and potential morbidity. Our findings were consistent with Pietriwicz et al study who found significantly higher homocysteine level in JIA patients compared to control group and even higher homocysteine level in polyarthritis group compared to oligo arthritis patients.18
Pathogenesis of juvenile idiopathic arthritis (JIA) includes increased inflammatory markers, homocysteine, lipids levels and inflammatory cytokines.19 It is hypothesized from a post mortem study that an excess of homocysteine may play a significant role in the development of atherosclerotic lesions.20
At present, there are many known risk factors for developing atherosclerosis. Some of them are amenable and may be modified, while some are non-amenable and cannot be modified; however, it is possible to identify groups at increased risk for cardiovascular diseases. Considering the fact that clinical consequence of the atherosclerotic process begins early in childhood but manifest during adult life, the introduction of appropriate preventive measures in children belonging to the risk group for cardiovascular disease and osteoporosis, is important. These measures may halt the development of the atherosclerotic process and other complications including osteoporosis at an early stage.
Conclusion
It is evident that a considerable number of JIA patients had hyperhomocysteinaemia considering the adult normal mean level as standard. Further study with larger sample size on new-onset JIA patients are recommended to explore the association between serum homocysteine levels and the disease.
AcknowledgementDeeply acknowledge to the JIA patients and their parents who participated in the study.
References
- Kliegman RM, Stanton BF, Schor NF, Geme JWS, Behrman RE. Nelson Textbook of Paediatrics. 20theditions. Philadelphia: Saunders Elsevier; 2016.
Doi: - Rees MM, Rodgers GM. Homocysteinemia: Association of a metabolic disorder with vascular disease and thrombosis. Thrombosis Research 1993; 7: 337-41.
Doi: - Osganian SK, Stampfer MJ, Spiegelman D, Rimm E, Cutler JA, Feldmam HA et al. Distribution of and factors associated with serum homocysteine levels in children. JAMA 1999; 281: 1189-96.
Doi: - Elshorbagy AK, Gjesdal CG, Nurk E, Tell GS, Ueland PM, NygardOTA. Cysteine, homocysteineand bone mineral density: a role for body composition? Bone 2009; 44: 954–58.
Doi: - van Meurs JB, Dhonukshe-Rutten RA, Pluijm SM, van der Klift M, de Jonge R, Lindemans J et al. HomocysteineLevels and the Risk of Osteoporotic Fracture. N Eng J Med 2004; 350: 2033-41.
Doi: - Casanueva V, Cid X, Cancino M, Cid L. Serum homocysteine in children and adolescents: Relation with family history of cardiovascular disease. Revista Medica de Chile 2003;131: 997-1002.
Doi: - Farhad M, Mehdi Q, Soheila N, Mohammad RR, Marjan S, Mojdeh S. Does Short-Term Low-Dose Methotrexate Treatment Affect Homocysteine Blood Level in Patients with Psoriasis? Iranian Journal of Dermatology 2009; 12: 9-12.
Doi: - Huemer M, Fodinger M, Huemer C, Sailer-Hock J, Falger A, Rettenbacher M et al. Hyperhomocysteinemia in children with juvenile idiopathic arthritis is not influenced by methotrexate treatment and folic acid supplementation: A pilot study. Clinical and Experimental Rheumatology 2003; 21: 249-55.
Doi: - Huemer M, Huemer C, Ulmer H, Crone J, Fodinger M, Falger J et al. No evidence for hyperhomocysteinemia or increased prevalence of genetic polymorphisms in the homocysteine pathway in patients with moderate juvenile idiopathic arthritis. The Journal of Rheumatology 2005; 32: 170-74.
Doi: - Ueland PM, Refsum H, Stabler SP, Malinow MR, Andersson A, Allen RH. Total homocysteine in plasma or serum: Methods and clinical application. Clin Chem 1993; 39: 1764-79.
Doi: - Robinson K, Mayer E, Jacobsen DW. Homocysteine and coronary artery disease. Cleveland Clinic Journal of Medicine 1994; 61: 438-50.
Doi: - Tonstad S, Refsum H, Ueland PM. Association between Plasma Total Homocysteine and Parental History of Cardiovascular Disease in Children with Familial Hypercholesterolemia. Circulation 1997; 96: 1803-08.
Doi: - Rahman SA, Islam MI, Talukder MK. Clinical aspects of juvenile idiopathic arthritis: extended experience from Bangladesh. American Journal of Clinical and Experimental Medicine 2013; 1: 20-23.
Doi: - Kunjir V, Venugopalan A, Chopra A. Profile of Indian Patients with Juvenile Onset Chronic Inflammatory Joint Disease Using the ILAR Classification Criteria for JIA: A Community-based Cohort Study. The Journal of Rheumatology 2010; 37: 1756-62.
Doi: - Shen C, Yeh KW, Ou LS, Yao TC, Chen LC, Huang JL et al. Clinical Features of Children with Juvenile Idiopathic Arthritis Using the ILAR Classification Criteria: A Community-Based Cohort Study in Taiwan. Journal of Microbiology, Immunology and Infection 2013; 46: 288-94.
Doi: - Gonçalves M, D’Almeida V, Guerra-Shinohara E M, Galdieri LC, Claudio AL, Maria OEH. Homocysteine and Lipid Profile in Children with Juvenile Idiopathic Arthritis. Pediatric Rheumatology 2007; 5: 1-7.
Doi: - Roubenoff R, Dellaripa P, Nadeau MR, Abad LW, Muldoon BA, Selhub J, Rosenberg IH. Abnormal homocysteine metabolism in rheumatoid arthritis. Arthritis and Rheumatism 1997; 40: 718-22.
Doi: - Pietrewicz E, Urban M. Early atherosclerosis changes in children with juvenile idiopathic arthritis. Polski Merkuriusz Lekarski 2007; 22: 211-14.
Doi: - Cassidy JT, Levinson JE, Bass JC, Baum J, Brewer EJ, Fink JCW et al. A study of classification criteria for a diagnosis of juvenile rheumatoid arthritis. Arthritis & Rheumatology 1986; 29: 274-81.
Doi: - McCully KS. Vascular pathology of homocysteinemia: implications for the pathogenesis of arteriosclerosis. American Journal Pathology 1969; 56: 111-28.
Doi:
Department of Paediatrics, Bangabandhu Sheikh Mujib Medical University, Bangladesh.
fakhrulbd77@gmail.com
 00000-0003-3061-1219
00000-0003-3061-1219
Submission
2018-08-26
Accepted
2020-04-01
Published
2020-04-01
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 46 No 1 (2020)
Section
Research Articles
Financial Support
None
Conflict of Interest
There was no conflict of interest.