ATM Atikur Rahman
Department of Paediatric Hematology and Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Momena Begum
Department of Paediatric Hematology and Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
C.S.H Kibria
Department of Paediatric Hematology and Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Mehnaz Akter
Department of Paediatric Hematology and Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Khurshida Azad Siddiqua
Ad-Din Hospital, Dhaka Bangladesh
Farzana Siddiqua
Department of Pharmacology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Choudhury Yakub Jamal
Department of Paediatric Hematology and Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Salahuddin Shah
Department of Hematology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Keywords: Rhabdomyosarcoma, Outcome, Treatment, Relapsed patients, Multimodality
DOI: 10.3329/bmrcb.v46i1.47464
Abstract
Background: Rhabdomyosarcoma (RMS) is a malignant tumor of mesenchymal origin, is the most common form of paediatric soft tissue sarcoma. It is the third most common solid tumor comprising 4.5% of all childhood cancer with an annual incidence of 4.5 cases per million children. There is so no statistical data on RMS in Bangladesh because no study has done in Bangladesh.
Objective: To evaluate the clinical characteristics and treatment outcome of children with rhabdomyosarcoma among tertiary care.
Methods: A retrospective study carried out analysing the medical records of 39 patients with rhabdomyosarcoma from the BSMMU tumor registry. Medical records of children with rhabdomyosarcoma were reviewed over a period of 6 years from June 2011 to May 2017. Most patients received multimodality therapy (chemotherapy, surgery, radiotherapy).
Results: The male female was ratio 1.2:1. More than half of cases presented with a mass at varying sites The predominant complaint 12.0% was pain. The primary site of disease was the head and neck in 46.0% followed by pelvis 40.0%. Pathologically most frequent histological subtype was in 46.0% embryonal rhabdomyosarcoma followed by alveolar rhabdomyosarcoma 23.0%, botryoid type 5.0%, spindle cell type 5.0% and unspecified 21.0%. At the time of diagnosis 64.0% of patients were TNM stage 3 next frequency is stage IV 23.0%. The survival rate from diagnosis to subsequent demise was poor – between 13 days and 3.5 years. The overall 5-year survival rate was 41.0% which is may be due to advanced stage of disease.
Conclusions: The majority of presentations were in the advanced stages of disease but sensitive to multimodality therapy. Poor survival rate is correlated with the advanced stage of the disease. The clinical characteristics of rhabdomyosarcoma at BSMMU Hospital are similar to worldwide countries, but not like developed countries. Further multicentre studies are needed to report our experiences with rhabdomyosarcoma.
Keywords: Rhabdomyosarcoma, Outcome, Treatment, Relapsed patients, Multimodality
Introduction
The majority of soft tissue sarcoma diagnosed in children are rhabdomyosarcoma (RMS) representing 6.0% of all childhood cancers.1,2 Most cases occur in children younger than 10 years.3 It is the third most common paediatric extracranial solid tumor after neuroblastoma and Wilms tumor. RMS is a malignant tumor of mesenchymal origin and is part of the group of small round blue cell tumors of childhood which include neuroblastoma, primitive mesenchymal tumors and lymphoma.21 RMS incidence is approximately 350 cases each year in the United States which corresponds to approximately 4.5 cases per 1,000,000 children per year.20,21
RMS is historically classified based on histopathologic features into distinct clinical subtypes - embryonal RMS (ERMS), alveolar RMS (ARMS), pleomorphic, and spindle cell and sclerosing RMS (ssRMS).22 ERMS represents the majority of cases and is associated with a favorable prognosis, while ARMS is more clinically aggressive due to a propensity for metastasis and recurrence.22
The two major histological subtypes embryonal and alveolar appear to be biologically distinct. Patients with embryonal RMS (ERMS) differ from those with alveolar RMS (ARMS) in terms of age of onset, primary tumor sites, propensity for metastasis and long term outcome. Successful treatment of RMS requires achievement of both local and systemic control of disease. Current treatment regimens incorporate surgery, chemotherapy and radiotherapy (RT). Using this multimodality approach the cure rates for RMS have steadily increased from only 25.0% in the 1970s to 70.0% in the 1990s.4-6 The results of IRS-IV emphasize that therapy for children with RMS should be risk directed and based primarily on tumor site, tumor histology, and extent of disease in addition COG treatment protocols for patients deliver risk-directed therapy based on histology and other prognostic factors.4,7 The local treatment protocol based on risk directed therapy.
The contribution of ethnic differences in biology, versus lack of delivery of adequate therapy, to this adverse outcome has not been studied. We conducted this retrospective study to evaluate the presentation, treatment, and outcome of patients with RMS treated in the pediatric Haemato-Oncology department, at a single tertiary care hospital in Bangladesh.
Materials and Methods
This was a retrospective review of medical records of patients with RMS seen at the Paediatric Haematology Oncology Department BSMMU from June 2011 to May 2017. Thirty nine (a small sample due to single centre study) patients were identified Information including patient age, sex, site of tumor, stage and clinical group, tumor histology, therapy, clinical course, and outcome were collected. Patients were identified by taking detailed history and did CT/MRI of site of lesions, biopsy, imaging and bone marrow done to detect distance metastases. This Study was approved by the Institutional Review Board (IRB) of the Bangabandhu Sheikh Mujib Medical University.
All newly diagnosed RMS, 0-18 yrs group children were included in this study. Age more than 18 years were excluded from this study.
reatment: In this study, treatment was using tri-modality treatment of chemotherapy, surgery and or radiotherapy as follow:
Chemotherapy: All patients received chemotherapy accordining to risk group. Low risk group A received 32 weeks of vincristine and actinomycin-D (vincristine 1.5 mg/m2 weekly, actinomycin-D 0.045 mg/Kg/day, day 1). Low risk group B and intermediate risk group received VAC for 43 weeks (vincristine 1.5 mg/m2 weekly, actinomycin-D 0.045 mg/ Kg/day, day 1 and cyclophosphomide 1.2 gm/m2 I.V with mesna every 21 days), high risk group received VAC alternating with ifosfamide 1.8 gm/m2 I.V day 1 to 5 with mesna and etoposide100 mg/m2 I.V day 1 to 5 every three weeks for 54 weeks. Relapsed patients from low risk group received VAC, intermediate and high risk group received 5 doses of ICE every 28 days (Carboplatine 450 mg/m2/day 1, with ifosfamide 1.8 gm/m2 I.V day 1 to 3 with mesna and etoposid 100 mg/m2 I.V day 1 to 3).
Definitive local control was attempted at weeks 10–15 of treatment with surgery, radiation therapy or combination of both. For radiation planning the gross target volume (GTV) used was the tumor volume defined by CT scan or MRI prior to any surgical debulking. This volume included clinically involved lymph nodes. An additional margin of 1.5–2 cm around the GTV was generated to create the clinical target volume (CTV) then an additional 0.5 cm margin was taken around the CTV to account for day-to-day setup variation. The total dose used was 50.4 Gy for gross disease, 45 Gy for orbital and eyelid sites, and 41.4 Gy for microscopic disease and sites of involved but resected lymph nodes. Completely resected alveolar histology tumors received 36 Gy. Clinically involved unresected lymph nodes received 50.4 Gy. The dose per fraction used was 1.8 Gy per fraction, 5 days per week and the technique was by three-dimensional conformal radiation therapy.
Response was evaluated by radiological imaging (CT or MRI) after 3-4 cycles of chemotherapy (weeks 9-12) then every 2-3 months. Survival was defined as the time interval from diagnosis to either death from any cause or last follow-up. Event-free survival was defined as time to disease progression, relapse or death from any cause.
Statistical Package for Social Sciences program (SPSS) was used for data management and analyses. Association between the different variables and the outcome was assessed using the Chi-square test or Fisher’s exact test as appropriate. Survival analysis was carried out and Kaplan Meier curves were constructed for the different groups. Statistical significance was considered at the 0.05 level.
Results
Thirty nine cases were included in this study. The age at diagnosis 7 days to 13 years, median age 5yrs. Male 22 (56.0%) and females 17 (44.0%). Most of the children presented with a mass (63.0%) at varying sites which was noticed 7 days to 3 months before consultation with a case presenting as late as 6 months. There were 22 (9%) patients who presented early within 2 weeks. The rest of the 22 patients presented late over a time period of 2 months to 6 months.
A number of cases presented with pressure symptoms (21.0%) especially due to bladder tumors with associated dribbling, urgency, poor stream and incomplete voiding. Pain was the predominant complaint in 9.0% of cases mostly in abdomen, leg and in eye. One patient presented with vaginal bleeding.
Delay in diagnosis was found in 8 of the 39 cases. Half of the cases had a period of delay of 3 weeks to one month. The rest had periods of delay of 6 weeks 2 months to 5 months and the longest being 6 months. Most of them presented and were treated as common paediatric problems namely otitis media, sinusitis, urinary tract infections.
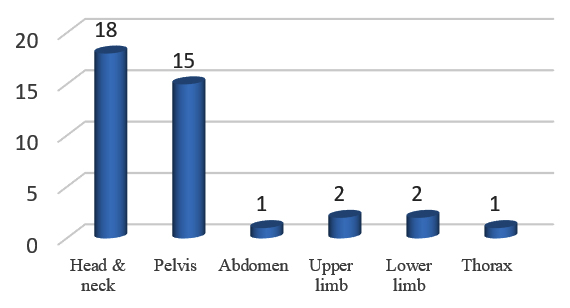
The primary site of disease was in the head and neck 18 (46.0%) and the pelvis (bladder, vagina, testicular and anal canal) 15 (40.0%). Less frequent sites were abdomen, upper limb, lower limb and thorax (Figure 1).
The commonest primary site of disease was the head and neck in 46.0% followed by the pelvis (bladder, vagina, testicular and anal canal) in 40.0%.
The most common histological subtype was Embryonal rhabdomyosarcoma in 18 patients (46.0%). The alveolar subtype accounted 9 (23.0%), botryoid 2 (5%), spindle cell 2 (5.0%) and other subtypes 8 (21%) (table 1).
| Pathological subtype | N= 39 | % |
|---|---|---|
| Embryonal | 18 | 46.15 |
| Alveolar | 9 | 23,07 |
| Botryoid | 2 | 5.12 |
| Spindle cell | 2 | 5.12 |
| Others | 8 | 20.51 |
25 (64.0%) were stage III at time of diagnosis, 9 (23.0%) at stage IV, 5 (12.8%) were stage II and there were no stage I (table I). The mean age of stage III patients was 6 years and in stage IV patients it was 7 years. There were 76% males in stage III and 24% males in stage IV. Females accounted for 69% of stage III and 31% of stage IV.
| Stage of disease at diagnosis | N=39 | % |
|---|---|---|
| Stage I | 0 | 0 |
| Stage II | 5 | 12.82 |
| Stage III | 25 | 64 |
| Stage IV | 9 | 23 |
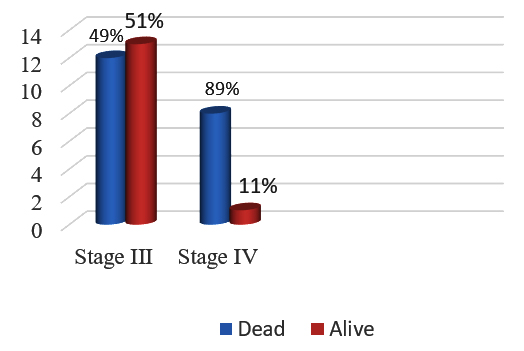
Regarding the histological subtypes in stage III were embryonal 71.0% and alveolar 60.0%. The stage IV subtypes were embryonal 29.0%, alveolar 40.0% (Figure 2).
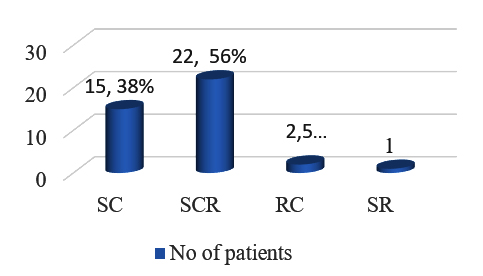
More than half of the patients 22 (56%) received multimodal therapy as shown in (Figure 3). This entailed surgery (biopsy or resection where possible) chemotherapy and radiotherapy (for patients with residual disease or as palliative care).
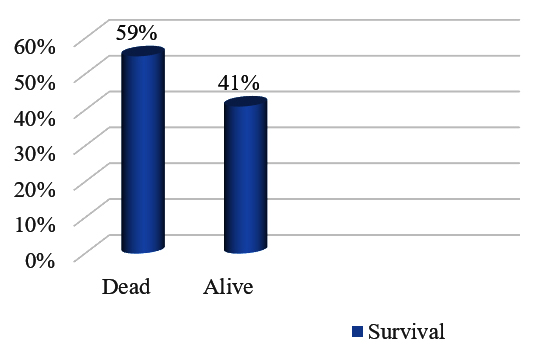
Survival duration was poor between 13 days and 3.5 years from diagnosis to subsequent demise. The overall 5 year survival rate was 45% (figure 3). This constituted 58% male and 29% female. The correlation between stage and survival is shown in (Figure 4) with 55% of survivors in stage III and 13% in stage IV
Discussion
Over the last three decades treatment outcome for patients with RMS has improved with intensive multimodal therapy which involves a combination of surgery, chemotherapy and radiotherapy.1,3-6 Despite advances in therapy 30.0% of children with RMS experience progressive or relapsed disease.7 There was a slight male predominance in our study which correlated positively with other reports in the literature. Francis et al in Nigeria had a two-thirds male predominance14. Previously study on RMS not done in Bangladesh and there is no published report.
Most (87.0%) of the rhabdomyosarcomas are found in the under 15-year age group.8 The head and neck and genitourinary systems are most often involved in the 2 to 6 year age groups.8 The median age of 5 years found in this study group of less than 15 years corresponds with Brown et al, which yielded similar results.9 Their age ranged from < 1 year to 14 years and their median age was 6.2 years.6 The primary site of disease in our study as well as with Brown et al, was the head and neck followed by the genitourinary system. This correlates positively with the age and primary site association as found in western literature. Francis et al differed with the literature and found that the extremities (50%) were the most common sites of disease.14 They also had a predominance of alveolar RMS which together with this site signifies a poor prognosis. Here only had 2 patients with this site of disease.
This study found a delay time to diagnosis ranging from 3 days to 6 months. The presenting symptoms can often mimic common childhood illness which is another factor delaying diagnosis. 1,5,8 This correlates well with the Nigerian study who showed that 100.0% of their study group also presented with a mass.14 The two most common subtypes embryonal and alveolar account for at least 80% of all rhabdomyosarcomas.8-9
Recent studies in the literature have reflected that embryonal RMS was three times more commonthan alveolar RMS.1,4 Results of the study show that embryonal RMS was indeed the more common histological subtype at 45.0% but the unspecified RMS subtype was the second commonest at 27.0%.
These histological subtypes have prognostic significance as well. Embryonal RMS tends to be a localized cancer that responds well to treatment and rarely spreads.8,10-11 Alveolar RMS tends to be aggressive and harder to treat with a poorer prognosis.10-12 In this study correlation between stage and histology indicated that 79.0% of the embryonal types were stage III as were 75.0% of the unspecified and 50.0% of the alveolar types.
Tumor histology is an important predictor of 5-year survival. IRSG III – IV found that alveolar RMS or undifferentiated sarcomas had a worse outcome with a 5-year failure free survival rate (FFS) of 5%.7,13 The 5-year survival rate for botryoid tumor was 64% and 26% for patients with embryonal tumors.7,10 The IRSG further identified prognostic factors within histological subtypes. The earlier the presentation and therefore the earlier stage or group within the embryonal tumors the better the prognosis.7,10
Early stages of disease (stage I and II) have survival rates of 70.0%.15Delay in presentation accounted for almost 48.0% of cases in this study leading to the majority of presentations being in the advanced stages of disease. Delay in diagnosis accounted for 24.0% of cases. Hessisen et al (2009) in their retrospective study in Morocco stated that 81.0% of cases had a 6-month or less delay in diagnosis.16
Approximately 91.0% of the patients were stage III and IV at time of diagnosis. This was due to late presentation in advanced stages of disease which played a major role in the poor outcome of the patients in this study subsequently leading to an overall 5-year survival rate of 45% in the availability of multimodal therapy.
Conclusion
The study finding suggest that recognition of early warning signs and public awareness could lead to earlier presentations and improve outcome. More study needed to compare with this study furthermore.
As the sample size was small and conducted at a single centre study. Further multicentre studies are suggested.
References
- Cripe TP, Gross S, Windle ML, Bergstrom SK, Petry PD, Coppes MJ. Rhabdomyosarcoma. Emedicine 2006; 4:1-10.
Doi: - Brown BJ, Oluwasola AO. Childhood rhabdomyosarcoma in Ibadan, Nigeria: 1984-2003. Annals of Tropical Paediatrics: International Child Health. 2006;26:349-355.
Doi: - Pappo AS, Anderson JR, Christ WM at el. Survival after relapse in children and adolescents with rhabdomyosarcoma: A report from the Intergroup Rhabdomyosarcoma Study Group. J Clin Oncol. 1999;17:3487-93.
Doi: - Meza JL, Anderson J, Pappo AS, Meyer WH. Analysis of Prognostic factors in patients with nonmetastatic rhabdomyosarcoma treated on intergroup rhabdomyosarcoma studies III and IV: the children’s oncology group. J Clin Oncol. 2006; 24:3844-51.
Doi: - Peters E, Cohen M, Altini M, Murray J. Rhabdomyosarcoma of the oral and paraoral region. Cancer. 1989;63:963-966.
Doi: - Hawkins D, Anderson JR, Paidas CN et al. Improved Outcome for Patients with Middle Ear Rhabdomyosarcoma: A Children’s Oncology Group Study. J Clin Oncol. 2001;19:3073-3079.
Doi: - Uba FA, Chirdan LB. Clinical characteristics and outcome of surgical treatment of childhood rhabdomyosarcoma: A 7 year experience. Afr J Paediatr Surg. 2008;5:19-23.
Doi: - Carli M, Colombatti R, Oberlin O et al. European Intergroup Studies (MMT4-89 and MMT4-91) on Childhood Metastatic Rhabdomyosarcoma: Final Results and analysis of prognostic factors. J Clin Oncol. 2004;22:4787-4794.
Doi: - Hessisen L, Kanouni L, Kili M et al. Pediatric Rhabdomyosarcoma in Morocco. Pediatr Blood Cancer. 2010;54:25-8.
Doi: - Adigun IA, Rahman GA, Buhari MO, Ogundipe KO, Omotayo JA. Pattern of Rhabdomyosarcoma in Nigerian Children. J Natl Med Assoc. 2008;100:906–09.
Doi: - Brown BJ, Oluwasola AO. Childhood rhabdomyosarcoma in Ibadan, Nigeria: 1984-2003. Annals of Tropical Paediatrics: International Child Health 2006;26:349-355.
Doi: - Pappo AS, Anderson JR, Christ WM at el. Survival after relapse in children and adolescents with rhabdomyosarcoma: A report from the Intergroup Rhabdomyosarcoma Study Group. J Clin Oncol. 1999;17:3487-93.
Doi: - Meza JL, Anderson J, Pappo AS, Meyer WH. Analysis of Prognostic factors in patients with nonmetastatic rhabdomyosarcoma treated on intergroup rhabdomyosarcoma studies III and IV: the children’s oncology group. J Clin Oncol. 2006; 24:3844-51.
Doi: - Peters E, Cohen M, Altini M, Murray J. Rhabdomyosarcoma of the oral and paraoral region. Cancer. 1989;63:963-966.
Doi: - Hawkins D, Anderson JR, Paidas CN et al. Improved Outcome for Patients with Middle Ear Rhabdomyosarcoma: A Children’s Oncology Group Study. J Clin Oncol. 2001;19:3073-3079.
Doi: - Uba FA, Chirdan LB. Clinical characteristics and outcome of surgical treatment of childhood rhabdomyosarcoma: A 7 year experience. Afr J Paediatr Surg. 2008;5:19-23.
Doi: - Carli M, Colombatti R, Oberlin O et al. European Intergroup Studies (MMT4-89 and MMT4-91) on Childhood Metastatic Rhabdomyosarcoma: Final Results and analysis of prognostic factors. J Clin Oncol. 2004;22:4787-4794
Doi: - Hessisen L, Kanouni L, Kili M et al. Pediatric Rhabdomyosarcoma in Morocco. Pediatr Blood Cancer. 2010;54:25-8.
Doi: - Adigun IA, Rahman GA, Buhari MO, Ogundipe KO, Omotayo JA. Pattern of Rhabdomyosarcoma in Nigerian Children. J Natl Med Assoc. 2008;100:906–909.
Doi: - Dasgupta R, Fuchs J, Rodeberg D. Rhabdomyosarcoma. Pediatr. Surg. 2016;25:276–283.
Doi: - Juan P, Gurria, Roshni D. Rhabdomyosarcoma and Extraosseous EwingSarcoma. Children. 2018; 5: 165.
Doi: - Celine C, Dorado, Garcia, Monika S, Anton G. Current and Future Treatment Strategies for Rhabdomyosarcoma. frontiers in oncology. 2019; 9,1458.
Doi:
Department of Paediatric Hematology and Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
atmrahmam1@yahoo.com
 0000-0002-6142-2528
0000-0002-6142-2528
Submission
2019-05-13
Accepted
2020-04-01
Published
2020-04-01
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 46 No 1 (2020)
Section
Research Articles
Financial Support
None
Conflict of Interest
None