Namkha Dorji
Department of Obstetrics and Gynaecology, Jigme Dorji Wangchuck National Referral Hospital, Thimphu, Bhutan.
Phurpa
Faculty of Postgraduate Medicine, Khesar Gyalpo University of Medical Sciences of Bhutan, Thimphu, Bhutan.
Birendra Pradhan
Department of Pathology and Laboratory Medicine, Jigme Dorji Wangchuck National Referral Hospital, Thimphu, Bhutan.
Mehriban Amatullah
Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Tasfia Mahmud
Sirajul Islam Medical College, Dhaka, Bangladesh.
Shirin Akter Begum
Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Keywords: Retroperitoneal mucinous cyst; Laparotomy; Histopathology; Ovarian tumour
DOI: 10.3329/bmrcb.v47i2.57784
Abstract
Background: Retroperitoneal cyst is a rare event with diagnostic and therapeutic challenges. It may remain asymptomatic or present with vague symptoms such as abdominal distension or pain. In the event of late diagnosis, it might develop complications like infection, perforation, haemorrhage and malignant transformation.
Objective: As there is not a single reported case from Bhutan, this is the first report to sensitise the clinicians so that they are aware about the rare possibility of this lesion.
Case: A 34-year-old woman presented with abdominal pain was diagnosed as ovarian tumour. During laparotomy, the mass was found to be a retroperitoneal cyst which was excised completely with intact capsule. The uterus, bilateral ovaries and fallopian tubes were normal. Histopathology confirmed that it to be benign primary retroperitoneal cyst.
Conclusion: Involvement of multidisciplinary team members would facilitate proper diagnosis and appropriate management of retroperitoneal cysts.Keywords: Retroperitoneal mucinous cyst; Laparotomy; Histopathology; Ovarian tumour.
Introduction
Retroperitoneal cysts are uncommon medical conditions with an ill-defined incidence.1 As there is no epithelium in the retroperitoneum, PRMC is an extremely rare tumour.2 They pose enormous diagnostic and therapeutic challenges for both the surgeons and radiologists due to their uncharacteristic clinical presentations ranging from being asymptomatic to vague abdominal pain or distention.1,3 Although, ultrasound, computerized tomography (CT) and magnetic resonance imaging (MRI) narrows the differential diagnoses yet they have inherent diagnostic limitations due to their overlapping imaging findings.4-7 Hence, retroperitoneal cysts are frequently diagnosed during laparoscopy or laparotomy.5 Histopathology remains to be the cornerstone for determining the ultimate diagnosis of retroperitoneal cysts.4 Among retroperitoneal cysts, primary retroperitoneal mucinous cystadenoma (PRMC) is a very rare benign tumour with an unclear histogenesis and biological behaviour.8 Thus, we present a case of retroperitoneal cyst which was diagnosed intraoperatively and subsequently confirmed to be a PRMC.
The Case
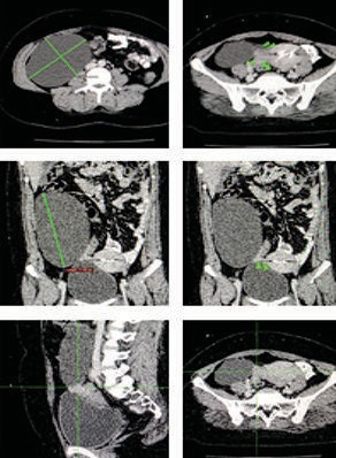
A 34-year-old woman was admitted to a local hospital (primary health centre) with abdominal pain for a month duration. The pain was felt in the upper abdomen, insidious in onset, colicky in nature without any identified aggravating or relieving factors. She had an episode of vomiting. She was apparently healthy woman without any significant medical disorders or any history of abdominal surgery. Ultrasound scan revealed cystic lesion measuring (14×8 cm) located anterior to pancreatic head. She was managed symptomatically and referred to a higher center for further workup for suspected pancreatic pseudocyst. On readmission to another hospital (secondary health care centre), intraabdominal cystic mass (10×10 cm) on right lumbar and right iliac fossa extending into the pelvis was noted by a general surgeon on physical examinations. CT scan done at Jigme Dorji Wangchuck National Referral Hospital (JDWNRH) revealed a well-defined cystic lesion (17.0×9.9 cm) occupying right flank and pelvic cavity (Figure 1).
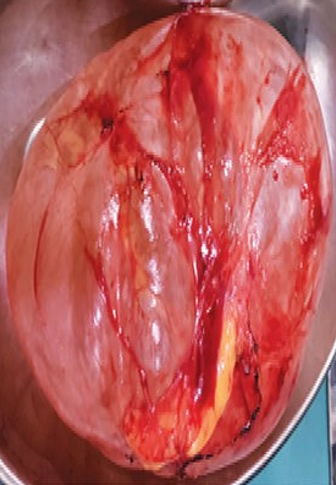
The lesion was not separated from the right ovary. Based on this CT scan findings suggestive of ovarian tumour, the case was referred to gynaecological oncologist for further evaluation. The tumour markers were done and showed as follows: beta HCG: <0.100 IU/ml, AFP: 6.31 ng/ml, CEA: 2.70 ng/ml, CA 125: 15.8 5 U/ml and CA 19.9: <0.600 U/ml. Ecchinococcus antigen was tested negative.With this clinical diagnosis of suspected ovarian tumour, gynaecological oncologist decided to perform diagnostic laparotomy and proceeded under general anaesthesia after informed written consent of the patient. Midline incision extending from above umbilicus to above symphysis pubis was made. There was a big retroperitoneal cyst (17×12×8 cm) in the right parabolic gutter (Figure 2).
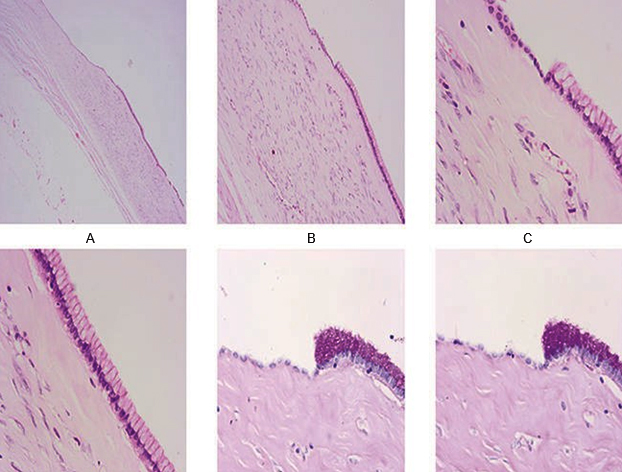
and displacing the ascending colon upwards and medially. The cyst was not connected with any nearby structures. The uterus, fallopian tubes and ovaries were normal in appearance which were left in-situ intact. Intraoperative consultation with general surgeon was done and decided for complete excision of cyst as it was benign looking. The cyst was excised with intact capsule and sent for histopathology report.Macroscopic examination revealed smooth external surface of cyst with congested vessels. Cut section showed unilocular cyst containing thin, clear serous fluid. Inner surface was smooth and no solid area seen with wall thickness of 0.1cm. Microscopic examination showed thin fibrous wall with focal calcification, lined by columnar epithelium. There was no evidence of atypia. Mucinous cystadenoma was diagnosed (Figure 3A-F).
On meeting face to face with patient and her family during follow up, they expressed their satisfaction and gratitude for the care given by medical team. They agreed to continue follow up.
She had an uneventful postoperative recovery and discharged home on postoperative third day. On review six weeks after surgery, her symptoms had subsided and wound healed.
Discussion
The masses that arise within the retroperitoneal space is called retroperitoneal cyst. It has no anatomical connection with any solid nearby organs.7 Their challenging clinical presentations create diagnostic and therapeutic dilemma for the clinicians. Cystic retroperitoneal masses could be either neoplastic or non-neoplastic, and one among later is primary retroperitoneal mucinous cystadenoma.4,8 The incidence of primary benign retroperitoneal cyst is unknown in Bhutan. As there is not a single reported case from Bhutan, this is the first report to sensitise the clinicians so that they are aware about the rare possibility of this lesion.
Retroperitoneal cyst presents with vague symptoms such as abdominal distension, features of intestinal obstruction.9 While one third are incidental detection. Other non-specific symptoms can include weight loss, back pain, swelling of lower limbs and referred pain to lower lips because of pressure effect on nearby structures. In this case, she had symptoms suggestive of subacute intestinal obstruction. These symptoms could possibly be due to displacement of ascending colon medially and cranially as noted during operation. Imaging studies such as ultrasound and CT scan are important to identify anatomical location, size and nature of the mass and its connection with nearby structures. CT scan helps to find the presence and thickness of the wall, septa, calcification, and fat.3,9 Accurate clinical information and familiarity with the most relevant radiologic features allows for appropriate lesion characterisation.7,10 In this case, symptoms presentation like subacute intestinal obstruction with examination finding of intraabdominal cystic mass (10×10 cm) on right lumbar and right iliac fossa extending into the pelvis may have contributed towards clinical confusion. Although, the CT scan was able to provide information on cyst size and location, its reporting as not separated from ovary created further diagnostic dilemma. There are reports where retroperitoneal mass is diagnosed as ovarian mass preoperatively.3 MRI may be useful in preoperative localisation and differentiation of retroperitoneal cyst (3,4).3,4 In this case, laparotomy was opted by patient without MRI as the patient wanted the mass to be excised and establish histological diagnosis.
Surgical intervention is indicated for a large symptomatic mass and when inherent complications like infection, perforation and malignancy are suspected.9-11 Image guided drainage of cyst can provide preoperative microbiological analysis and exclude malignancy as well as symptom relief (1). There are instances where the mass is detected incidentally and multidisciplinary team had come to common consensus of keeping the mass in-situ without disturbing, but had to remove by the same team as the patient insisted on removal.3 As in this case, unexpected finding of retroperitoneal mass, gynaecologists are challenged on what would be the next most appropriate action.5 Depending on the availability of expertise and facilities, either laparotomy or laparoscopy can be used to excise the cyst. Complete excision of the cyst is preferred over marsupialization or simple fenestration. Histology of cyst wall is mandatory. Intraoperative frozen section is advisable if partial resection is planned.6 In this case, as the cyst was macroscopically benign looking and complete excision of cyst without disrupting the cyst wall was possible, intraoperative frozen section was not done. Histology and immunohistochemistry confirmed mucinous cystadenoma. It is a homogenous and well-defined unilocular cysts detected in woman with normal ovaries. There is no specific characteristic appearance of mucinous cystadenoma over other retroperitoneal cysts on CT scan.12
Conclusion
Benign primary retroperitoneal mucinous cystadenoma in adult is an uncommon presentation of abdominal pathology. The vague symptomatic presentation creates difficulty in clinical diagnosis. Imaging studies such as ultrasound, CT scan and MRI play a crucial role in defining these lesions preoperatively. Intraoperative inter-departmental consultation and complete surgical excision is the cornerstone of treatment for symptomatic and complicated cases. Histopathology confirms final diagnosis which is useful for further management and follow up decisions.
Acknowledgments
We thank Dr Thukten Choiphel, General Surgeon, JDWNRH for his second opinion during the surgical excision and Dr Tashi Gyeltsen, Radiologist, JDWNRH for his valued opinion on CT scan.
References
- Morotti A, Busso M, Barozzino MC, Cinardo P, Angelino V, Familiari U, et al. Detection and management of retroperitoneal cystic lesions: A case report and review of the literature. Oncol Lett. 2017;14:1602-08.
- Paraskevakou H, Orfanos S, Diamantis T, Konstantinidou A, Patsouris E. Primary retroperitoneal mucinous cystadenoma. A rare case with two cysts and review of the literature. Hippokratia. 2014;18:278–81.
- Vilos AG, Vilos GA, Marks J, Pollett A. Retroperitoneal Pelvic Cyst: A Diagnostic and Therapeutic Challenge. J Obstet Gynaecol Canada [Internet]. 2013;35:164–7.
DOI: 10.1016/S1701-2163(15)31022-7 - Mota MMDS, Bezerra ROF, Garcia MRT. Practical approach to primary retroperitoneal masses in adults. Radiol Bras. 2018;51:391–400.
- Vilos GA, Vilos AG, Hollett-Caines J, Abu-Rafea B, Jacob GP, Ettler H. Retroperitoneal pelvic tumours in women: diagnostic and therapeutic challenges. Facts, views Vis ObGyn. 2020;11:299–306.
- Renzulli P, Candinas D. Symptomatic retroperitoneal cyst: A diagnostic challenge. Ann R Coll Surg Engl. 2009;91:10–2.
- Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, et al. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004;24:1353–65.
- Pesapane F, Van Renterghem S, Patella F, De Visschere P, Villeirs G. A case report and a literature review of primary retroperitoneal mucinous cystadenoma: The importance of imaging in diagnosis and management. Futur Oncol. 2018;14:2923–31.
- Ali D, Sarwar MZ, Manzoor F, Naqi SA. Benign idiopathic retroperitoneal cyst: A case series of three patients. Int J Surg Case Rep [Internet]. 2019;61:210–3.
DOI: 10.1016/j.ijscr.2019.07.050 - Mitura K, Mikolaj R, Alicja M. An atypical site of a retroperitoneal epidermoid cyst in a middle-aged woman. Int J Surg Case Rep [Internet]. 2013;4:85–7.
DOI: 10.1016/j.ijscr.2012.10.008 - Bakker RFR, Stoot JHMB, Blok P, Merkus JWS. Primary retroperitoneal mucinous cystadenoma with sarcoma-like mural nodule: A case report and review of the literature. Virchows Arch. 2007;451:853–7.
- Zaheer A, Pokharel SS, Wolfgang C, Fishman EK, Horton KM. Incidentally detected cystic lesions of the pancreas on CT: Review of literature and management suggestions. Abdom Imaging. 2013;38:331–41.
Jigme Dorji Wangchuk National Hospital, Thimphu, Bhutan.
namji2002@gmail.com
 0000-0003-3594-3159
0000-0003-3594-3159
Submission
2021-03-15
Accepted
2021-06-30
Published
2021-08-01
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 47 No 2 (2021)
Section
Case Report
Financial Support
None
Conflict of Interest
None